By Amartya Pradhan and Manusmriti Agarwal


Coronavirus disease 2019, or COVID-19, has been declared a pandemic by the World Health Organization (WHO) on March 11, 2020, following its outbreak in November 2019. Preliminary studies trace back to a zoonotic transfer of SARS-CoV-2 from bats (reservoir host) to humans in Wuhan, China. Since then, it has managed to indiscriminately affect all humans living across 200+ countries and territories in some way or the other, ‘without batting an eye’. COVID-19 is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Since the outbreak of COVID-19, scientists have been studying its epidemiology and underlying mode of transmission from one person to another. There have been conflicting reports about such mechanisms of transmission leading to a lot of confusion. Enormous efforts have been and are being made to stop its spread and mitigate the chances of infection to an uninfected person. Many believe that a partial or a complete lockdown will be beneficial in arresting its spread. Others suspect that by allowing the virus to infect a majority of the population, large numbers of people develop an immunity against the virus, (also known as herd immunity), and hence stop such infections in the future. Let us look into each school of thought with examples through graphs (Fig. 1).
Fig. 1: Graphs represent a normal distribution for the daily number of cases. The area shaded in magenta represents the projected number of daily cases when no social distancing is practiced, whereas areas shaded in pink lines show the number of cases when proper hygiene and social distancing are practiced. (Image: © CDC)
When there is no intervention by the people/government, i.e. when everything goes as it was before the outbreak, we see that there is a sudden surge in the number of cases. In this scenario, the infection sweeps through a significant portion of the population and the number of cases drops in a relatively shorter period of time. However, it burdens the healthcare system and supply chains of critical pieces of equipment. Such crashing of healthcare services and supply chains were evidently observed in the New York State of the US between March and May of 2020. This type of distribution is dependent on the fact that recovered patients develop immunity against the pathogen, and that the pathogen itself doesn’t mutate rapidly to infect recovered patients again. On the other hand, when we practice hygiene and social distancing, it affects a relatively smaller population. Here, the rate of spread of infection is slacked off, which is oftentimes known as ‘flattening the curve’. This approach takes a much longer time to cease the spread of infection. Having said that, it doesn’t burden the health system and supply chains. Furthermore, absolute mortality is comparatively lower than the former approach. New Zealand demonstrated the best example of this process. It is interesting to look at how they were able to control the COVID-19 epidemic in their country; declared themselves COVID-19-free without compromising on their healthcare system. This approach is contingent upon proper social distancing and hygiene practices. As of Jun 16, 2020, COVID-19 epidemiology in India exemplifies that despite a lockdown in place, improper distancing practices lead to an exponential increase in daily new cases.
Fig. 2: Graphs show the daily number of cases in (left to right) New York (US), New Zealand, and India, respectively. Please note that the given graphs are not normalized against time and the number of daily cases. Hence, given trends are not superimposable. (Image: COVID-19 Tracker, https://bing.com/covid).
Irrespective of either approach, personal hygiene and safety are important if you don’t want to end up in a hospital, or in the worst case, a mortuary! With regard to safety and protection, there are guidelines by WHO and local health authorities. You can find links to these pages in the reference section. Here we will focus on how to follow those procedures, the correct way, and aim to bust myths and clear confusion around COVID-19.
Health authorities focus on wearing masks and gloves when outside. However, there have been cases where despite following such precautions, people end up getting the disease. But how does that happen? How do healthcare professionals and researchers get away by wearing the same masks and gloves?
The answer lies in the way we use masks and gloves. So here is an illustration of how a lack of precaution helps to spread COVID-19. Imagine that you’ve got a brand new pair of gloves and masks and you want to go outside for shopping. You put your gloves and mask on, and head out in your car. You enter a shopping complex and grab a cart for yourself. The cart handle is housing our villain, the SARS-CoV-2! You touch the handle, then grab some groceries, pay your bill, get back into your car, go home and discard your mask and gloves. A couple of days later you and your family end up with COVID-19. Oops! What? How did that happen?
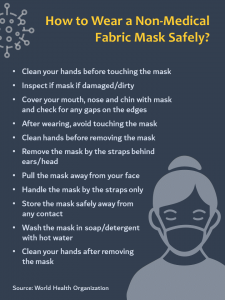
Let’s go back in time and revisit what could have been wrong. Now imagine SARS-CoV-2 as chocolate syrup and the cart handle is covered with it. So you are shopping, and you check your mobile to refer to your shopping list. There you go! You have your phone covered in syrup! Now you get your wallet and pay with your card. Now you’ve got syrup on it. While walking to your car, you call your sibling if they need something to eat. Oops! Did you realize that now you have got that chocolate on your cheeks and ear? Gross! Now you reach home. But your car steering wheel still has that chocolate syrup on it. Now you throw masks and gloves; you have clean hands but the virus is still there on your face, your mobile, and that darn steering. Now I think it is easy to imagine how you bite your nails after touching your phone. Your sibling decides to steal your card and buy new headphones online. Your parents drive that car to their office. I hope now you know how you and your family end up getting infected with SARS-Cov-2.
To conclude, it is important to wear gloves and masks. But it is more important not to touch your face. It is also crucial to consistently sanitize your hands, disinfect your mobile, or anything which is touched frequently. We researchers never touch our phones and face while working with bacterias or viruses. Practicing such simple procedures can save you and others from COVID-19 and probably other diseases.
Demystifying COVID-19
Scientific study suggests that spike (S)-protein of SARS-Cov-2 binds to the angiotensin-converting enzyme-2 (ACE-2) receptor expressed on a plethora of tissues including those in the upper and lower respiratory tract (Fig. 3). This interaction paves the way for the virus to invade human tissues. Interestingly, ACE-2 receptors are upregulated in individuals with smoking habits, and the pre-existing condition of chronic obstructive pulmonary disease (COPD). Hence, these groups are vulnerable and may exhibit exacerbated responses to the disease.
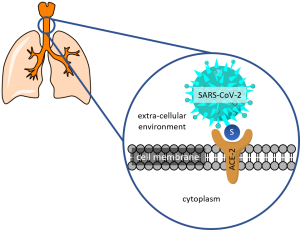
Fig. 3: Representative schematic showing the interaction of S-protein of SARS-CoV-2 with ACE-2 displaying cells in the respiratory tract.
We have lived through several outbreaks in the last 2 decades. The H1N1 influenza, Ebola, Zika, SARS-MERS pandemic all originated in the life form of a teeny tiny virus and yet COVID-19 proved to be the only one capable of scaring the entire world into their homes and lockdowns still subject to extension in major parts across the globe. The uncertainty and lack of complete understanding about the SARS-COV-2 virus and its transmission across vectors and human hosts alike seep fear into the everyday lives of each and everyone as we find ways to grapple with this singular moment in history while anticipating an end to this nightmare. What makes the current scenario so unique and intriguing? Apart from the possibility of the virus reaching every single human being and initiating the manifestation of COVID-19 in the form of its typical symptoms, the pandemic has also displayed the ability to play with the minds of the masses. While the experience of fear is but natural, paranoia, and feelings of emotional isolation resulting from social distancing and quarantining must be avoided to curb the surge of a potential mental health crisis during and post COVID-19.
Given the connectedness of the entire globe today courtesy technology, we have been able to prevent and postpone experiencing a complete halt to our work and information overload. While internet access and online proceedings remain a privilege in many parts of the world, a lack of understanding promotes fear amongst every human being without discrimination as COVID-19 gains passport and increasing momentum across human habitation worldwide. Along with the spread of COVID-19, rumors and myths have traveled faster adding to the fear and uncertainty around the existing conundrum rather unnecessarily.
‘‘Nothing in life is to be feared, it is only to be understood. Now is the time to understand more, so that we may fear less“-
drawing inspiration from Marie Curie, let’s get a hold of all the hoax and myths mystifying the COVID-19 situation and tackle them through understanding backed by facts.
Misleading Myth #1 Coronavirus is spreading rapidly and is the cause of the COVID-19 pandemic.
Busted!
The term coronavirus implies a large family of viruses known to cause respiratory illnesses across a wide spectrum of severity; however, it is only a recently discovered virus of this family, known as SARS-COV-2 that is responsible for the COVID-19 pandemic. The rate of spread of this particular virus is rapid through human contact (in the form of droplets transmitted while speaking/coughing/sneezing from nose and mouth) and contact with infected surfaces; however, the rate of spread of disease despite being rapid is dependent on various factors like immunity and vulnerability due to lifestyle and may create asymptomatic carriers out of individuals instead of patients.
Misleading Myth #2 The manifestation of COVID-19 resembles common cold and flu with respect to symptoms.
Busted!
While most common symptoms of COVID-19 are similar to those of common acute respiratory illnesses and the common cold, like fever, dry cough, and tiredness, there are other symptoms that as more research is being carried out and diversity is being observed in more and more patients.
Less common symptoms that are experienced by infected individuals are aches and pains, difficulty in breathing, nasal congestion, headache, conjunctivitis, sore throat, diarrhea, loss of taste or smell, or a rash on skin or discoloration of fingers or toes. These may be experienced mildly and may appear gradually.
Misleading Myth #3 Only the aged population is vulnerable to contracting COVID-19.
Busted!
Evidence suggests that SARS-CoV-2 doesn’t discriminate on the basis of age, or individual’s pre-existing conditions like diabetes. In other words, COVID-19 can happen to anyone! However, vulnerability groups including individuals with compromised immunity, smokers, diabetics, individuals with high blood pressure and borderline sugar levels, and individuals with a stress-prone lifestyle, are more prone to manifest severe symptoms. Hence, these individuals, if infected, might suffer more and have their lives at risk compared to non-vulnerable individuals.
Misleading Myth #4 Masks are reusable.
Busted!
You must never reuse marks, specifically surgical masks. These masks should not be worn for prolonged periods as it becomes damp and creates a niche for microbial growth. You must discard surgical masks safely. On the other hand, dry fabric masks (masks made of clothes) can be reused, but only after cleaning them with thorough detergents.
Misleading Myth #5 Hand sanitizers contain alcohol, so consuming alcohol will prevent COVID-19.
Busted!
The alcohol content in hand sanitizers is generally about 70%, whereas that in hard-drinks is on an average of about 40%. Consuming beverages with high alcohol content may damage our internal organs, and is highly dangerous. Furthermore, hand sanitizers are used externally and not consumed. In short, drinking alcohol is injurious to health and it doesn’t protect us against the virus. The best way to prevent the disease is to keep away from infected individuals, washing your hands regularly and avoid touching your face.
Misleading Myth #6 Antibiotics are effective in treating COVID-19.
Busted!
Antibiotics work against bacteria, not viruses. However, you may be prescribed one by the doctor on suspected bacterial co-infection due to compromised immunity. Hence, consuming antibiotics without a doctor’s recommendation will not be of any help, and may aid harmful bacteria in your body to acquire antibiotic resistance.
The question that now comes into being is how to survive the side-effects of the pandemic on our minds once we have mitigated the precautions and practice of isolation. Especially for healthcare professionals, stress and anxiety can occupy a major part of their routine. It has become a necessity to equip ourselves with certain ammunition against the fear and stress that this pandemic has brought with it.
Last but not the least, taking all the needful precautions as already mentioned should assure you and leave no room for paranoia and fear. Rest assured by following the mandate against the outbreak and playing your part in curbing the pandemic.
Immediate professional medical assistance and guidance are strongly recommended and advised for individuals experiencing mild fever, cold, cough, and other COVID-19 related symptoms. Professional psychological support and medical opinion are suggested in the case of mental health-related issues.
Resources:
https://www.drugwatch.com/health/how-to-deal-with-anxiety/
References
About the Authors
Amartya Pradhan was a Khorana Scholar’19 and is currently a 4th year B.E. (Biotechnology) student at the Netaji Subhas University of Technology, New Delhi, India.
Manusmriti Agarwal was a BEST Fellow’19 at IISc, Bangalore, and is currently a 4th year B.E. (Biotechnology) student at the Netaji Subhas University of Technology, New Delhi, India.
Both the authors are recipients of recognition from Schrödinger Inc. and membership of the American Chemical Society for their work and protocol on in silico antibody affinity maturation via computationally designed site-directed mutagenesis.